A staggering one-third of the global population may harbour metabolic dysfunction associated fatty liver disease (MAFLD). This burgeoning, obesity-related health crisis is projected to escalate, with obesity rates expected to jump from 15% in 2023 to ~25% by 2035.
Metadvice stands at the forefront of this challenge, leveraging AI to empower clinicians in managing the complex web of chronic diseases, particularly where metabolic and cardiovascular disorders intersect. In this blog, we draw on new evidence to explore how Metadvice technology can address this growing disease area.

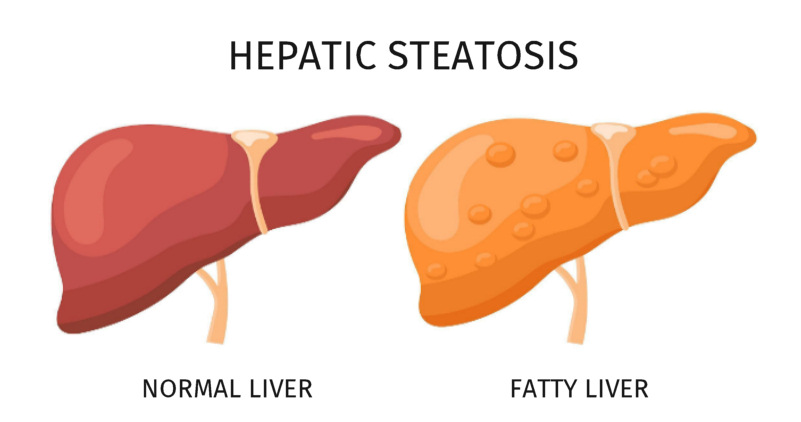
Myriad health implications of fatty liver
Hepatic steatosis is a prevalent and under-diagnosed condition closely associated with excess adiposity. Complications in a substantial minority of affected individuals include fibrosis and inflammation, conferring risks of cirrhosis and hepatocellular carcinoma. With the global prevalence of alcohol use disorders at 4.1%, the risks are magnified for those also battling obesity, underscoring the need for nuanced healthcare strategies.
‘In the battle against the silent epidemic of fatty liver disease, Metadvice identifies risks early and drives targeted patient management.’
Dr Andrew Rut, Metadvice CEO.
According to Prof. Andrew Krentz, Head of Metadvice’s Cardiometabolic Division, hepatic steatosis is now regarded as a multi-system disorder that is part of the insulin resistance-metabolic syndrome continuum. Establishing the diagnosis requires exclusion of alternative causes of chronic liver disease, e.g. viral hepatitis. Genetic variants that predispose to hepatic steatosis are recognised. Differentiation from chronic liver disease primarily attributable to alcohol excess relies on self-reported history of alcohol consumption. Recent evidence suggests that hepatic steatosis may predict the development of atherosclerotic cardiovascular disease (ASCVD) independently of other components of the metabolic syndrome. Thus, the rising incidence of fatty liver disease poses a threat to cardiovascular health across the globe. To date, no pharmacotherapeutics have been approved for the treatment of the progressive form of hepatic steatosis, i.e., metabolic associated hepatic steatohepatitis (MASH). Strategies for prevention and management are currently directed towards modifiable cardiometabolic risk factors.
The risk of adiposity-associated cardiometabolic disease, including hepatic steatosis, increases at lower levels of adiposity in South and East Asian populations. A recently published paper from Korea illustrates this point with a mean body mass index of ~25 kg/m2 across subgroups with steatotic liver disease. This paper, based on an adult cohort identified from a national screening programme, stratified steatotic liver disease according to recently redefined diagnostic criteria that incorporate components of the metabolic syndrome. The presence or absence of hepatic steatosis was ascertained using non-invasive methodologies. During a median observation period of 9 years, individuals with steatotic liver disease had a higher risk of developing ASCVD. A male preponderance of ASCVD risk was observed. Two major subtypes – metabolic dysfunction associated steatotic liver disease (MASLD) and metabolic dysfunction-associated steatotic liver disease with increased alcohol intake (MetALD) – were associated with a higher incidence of ASCVD. The investigators propose that cardiometabolic risk factors and alcohol consumption may additively elevate the risk of ASCVD. Of note, in this study population, stroke was more closely associated with hepatic steatosis than coronary heart disease. The investigators conclude that their observations validate the new diagnostic criteria for hepatic steatosis while offering the prospect of more granular risk stratification and improved strategies for prevention.
Metadvice: Turning the Tide on Cardiometabolic Risk
Dr Andrew Rut, CEO of Metadvice, adds: ‘Metadvice applies the principles of precision medicine to the diagnosis and management of chronic, often multi-morbid, disorders. Using proprietary neural networks trained on clinical guidelines, Metadvice interrogates electronic medical records to provide personalised evidence-based therapeutic recommendations. Metadvice helps to identify high risk patients early and ensure that appropriate and targeted intervention is implemented early to mitigate the long-term of multi-morbid cardiometabolic disorders. The benefits are thus manifold – being conferred to patients, clinicians and healthcare providers.’
‘The healthcare industry has been slow to adapt to AI, but Metadvice’s technology is the long-awaited disruptor. Beyond being mere management tools, our AI platforms are designed to predict disease trajectories and identify preventative strategies, ushering in a new era of healthcare where conditions like hepatic steatosis are not just controlled, but anticipated and circumvented. This heralds an era where diseases like hepatic steatosis won’t just be managed—they’ll be predicted and prevented.’
REFERENCE
Moon JH et al. Metabolic dysfunction-associated steatotic liver disease increases the risk of incident cardiovascular disease: a nationwide cohort study.
eClinicalMedicine 2023. https://doi.org/10.1016/j.eclinm.2023.102292
AK November 2023
